3 Common Health Emergencies You Should Prepare For

Have you ever came across an emergency situation where someone suddenly just drops and become unconscious? Or maybe you've even crossed paths with a person who had an acute severe pain in their chest. Perhaps, you know someone dear to you who experienced these things, and you didn't know what to do...
Being aware of what type of health emergencies that are likely to occur is important. This helps you to quickly identify the problem at hand, then think of the best solutions.
I've experienced seeing a lady on the train get into a fit. I was only 18 years old but I knew CPR and first-aid which helped me to not flinch and act calmly. I took note of the time, then pressed the emergency button and communicated the situation clearly and calmly. The entire train halted; we got the lady out as I instructed a man to call the ambulance. Thankfully, we had a trained doctor around who managed to assess her condition and intervened appropriately before the paramedics arrived.
Imagine this happened to you too... Do you know what to do? If you do, you could very well be saving one precious life. Just like how we saved the lady on the train.
Here are the 3 common health emergencies that you should prepare for and how.
1. Fits/Epileptic Seizures Emergency
This happens unexpectedly and it gets pretty violent too. The seizures are strong, uncontrollable, and abrupt. The sight of it can put you to a state of shock, and you might go blank in your head.
Here's what you can do:
- Stay calm (you do know what to do)
- Remove any dangerous objects around or move the person somewhere safe
- Take note of the time so that you can report to the paramedics when they arrive
- Let the episode end but stay with them
- Don't hold them down (they're unconsciously using close to maximum strength -- keep a distance unless you want to get sucker-punched)
- Don't put anything in their mouths (they won't bite their tongue off, but they might bite your finger off)
- Call an ambulance after 5 minutes of continuous seizure or they have difficulty breathing after the seizure has stopped
- Gently pry open and check if airways are blocked
- Turn them to a recovery position after seizure ceased, if not stay with them until the ambulance arrives
2. Bleeding Emergency
An open wound or cut, no matter how small, can cause some sort of bleeding. If not properly cared for, these wounds (especially the bigger ones) can lead to infection and even decay.
The concept of putting a stop to bleeding from minor cuts to deep lacerations is similar. The following steps are the fundamental first-aid procedures that you can apply.
- Apply direct pressure onto wound with a clean cloth, tissue, or gauze until bleeding ceases
- Add on more layers of cloth if the previous one is soaked, and do NOT remove the blood-soaked cloth
- Elevate the bleeding limb above the heart (if possible) -- this helps to slow the bleeding
- Wash hands prior to applying first-aid
- Clean wound with warm water and soap, rinse thoroughly
- Apply antibiotic cream and protect with a sterile bandage
Seems like second nature, right? Here's the meat and potatoes; how to react to a more serious bleeding situation.
When the wounds are deep or the edges of the skin are jagged and gaping open -- Call a doctor.
If the wound is on the face -- Call a doctor.
When the wound displays signs of infection (redness, thick discharge, or even a fever) -- Call a doctor.
If the area around the wound feels numb -- Call a doctor.
And the last segment of first-aid for bleeding, the severe situations, you should call 911.
Such situations include:
- Bleeding is severe
- Internal bleeding suspected
- Wound at the abdominal or chest
- Bleeding cannot be stopped even after 10 minutes of firm and steady pressure
- Blood is spurting out from the area of injury
3. Stroke and Heart Attack Emergency
Strokes
Strokes happen when either one of these occurs to a person.
- An artery is blocked (ischemic stroke)
- A blood vessel ruptures and bursts (hemorrhagic stroke)
However, in some cases, these major strokes don't happen without a warning -- Transient Ischemic Attack or TIA.
Other warning signs of a stroke are:
- Weakness and numbness, even paralysis on one side of the body (face and/or limbs)
- Vision is blurred, especially if it only affects one eye
- Slurring of speech
- Sudden difficulty in swallowing
- Loss of balance
- Sudden severe headaches that don't feel familiar
Heart Attacks
About 610,000 people die because of a heart attack every year in the United States. This number makes up a whopping 25% of the cause of death in the US. Myocardial Infarction (MI) or heart attack occurs when the blood flow to the heart is blocked via the coronary arteries. This blockage is caused by the build-up of cholesterol, fats, and other substance, eventually creating a plaque.
Signs and symptoms of a heart attack are:
- Pressure, tightness, pain, or a squeezing or aching sensation in your chest or arms that may spread to your neck, jaw or back
- Nausea, indigestion, heartburn or abdominal pain
- Shortness of breath
- Cold sweat
- Fatigue
- Lightheadedness or sudden dizziness
What You Can Do To Help
When dealing with a stroke or heart attack situation, you can follow these simple steps that are easy to remember and recall.
DRSABCD:
D: check for Danger
Ensure that the affected person, you, and others are safe and not vulnerable to any danger. Dangerous elements can include water, metal, flammable or explosive items, sharp objects, etc.
R: check Response
Call the person and squeeze their hand/arm, or shake them to elicit a response. If they responded, you can turn them over to a recovery position. If they did not respond, means that they are unconscious, and you can proceed to the next step.
S: Send for help
Get someone to call the ambulance and retrieve a defibrillator (AED).
A: check the Airway
Open the person's mouth and tilt his/her head back slightly. Check for any obstruction, vomit, or choking hazard. To remove the substance, turn the person to recover position and allow the obstructing fluid to flow out completely. Remove remaining substance with your fingers.
Recovery Position
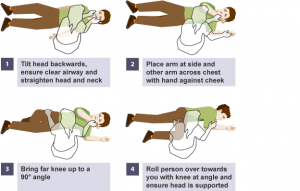
- Kneel beside the person.
- Put their arm that’s farthest from you out at right angles to their body.
- Place their nearer arm across their chest.
- Bend their nearer leg up at the knee; the other leg should be straight.
- While supporting their head and neck, roll the person away from you.
- When they are on their side, keep their top leg bent at the knee, with the knee touching the ground.
B: check for Breathing
You can do so by seeing if the chest rises and falls or not, feeling the breath on your cheek, or hear the sound of breathing. If the person is breathing, wait for help while ensuring the person is in the recovery position.
If there's no sign of breathing, the person will need you to perform cardiopulmonary resuscitation (CPR).
C: CPR
- Turn the person onto their back.
- Kneeling beside the person, give 30 chest compressions on the lower half of the breastbone. Use 2 hands with the fingers interlocked.
- Then tilt the head backwards, lift the chin and give 2 mouth-to-mouth breaths while pinching the nose shut.
- Keep alternating between 30 compressions and 2 breaths until the person shows signs of life or medical help arrives.
D: Defibrillation
Follow instructions calmly as the voice of the AED prompts.
